Some states are hesitant to cover the popular drugs.
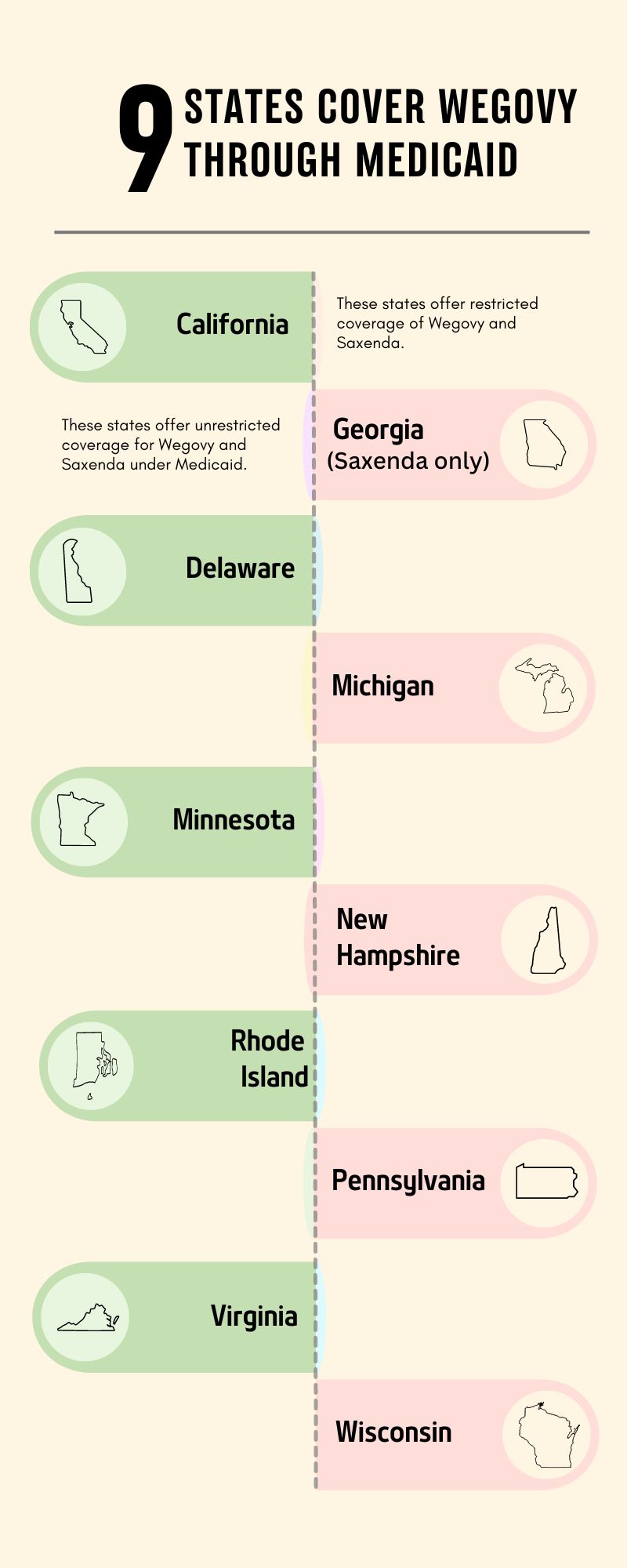
Weight loss drugs have soared in popularity; while some states have been hesitant to cover them, others have not. A recent JAMA study found that five states offer unrestricted coverage of GLP-1 drugs Wegovy and Saxenda that were approved for weight loss.
The data from this study comes from formularies for 47 state Medicaid programs from the first quarter of 2023.
The study found that a total of ten states cover Saxenda or Wegovy for weight loss, while five of those states offered restricted access through barriers like prior authorization, non-prefered status, or step therapy.
Some GLP-1 drugs approved for coverage to treat diabetes such as Ozempic, Victoza or Trulicity, are covered in 39 states.
Some states are hesitant to cover these popular drugs because of the hefty $15,000 price tag that accompanies them.
As 2023 these five states offer unrestricted coverage to Wegovy and Saxenda under Medicaid:
California
Delaware
Minnesota
Rhode Island
Virginia
These five states offer restricted coverage of Wegovy and Saxenda:
Georgia (Saxenda only)
Michigan
New Hampshire
Pennsylvania
Wisconsin
Marie DeFreitas is the finance editor for HealthLeaders.
